In this 2-part series, we will discuss the underpinning mechanisms of Tendon Neuroplastic Training and when it may be appropriate to use in practice.
Tendinopathies represent a significant injury burden in both athletic and general populations. In many instances, there is persistent or recalcitrant symptoms, especially when tendon capacity is not improved. We lack objective measures clinically that would link tissue pathology to the patient’s painful presentation and we know that the presence of tendinosis on imaging does not correlate well with pain. Therefore, we are restricted to improving tendon capacity via progressive loading while trying to mitigate the effects that pain may have on rehabilitation compliance.
In 2015, Ebonie Rio described a novel rehabilitation technique, Tendon Neuroplastic Training (TNT), that had the potential to significantly reduce the pain in tendinopathy by combining strength training with an audio or visual cue. This has shown preliminary benefits for patellar tendinopathy and lateral elbow tendinopathy with the notion that this may be applicable in other areas of the body. However, in order to effectively apply these techniques, which includes being able to describe this and get buy-in from an athlete or patient, you need to understand the underlying theoretical framework.
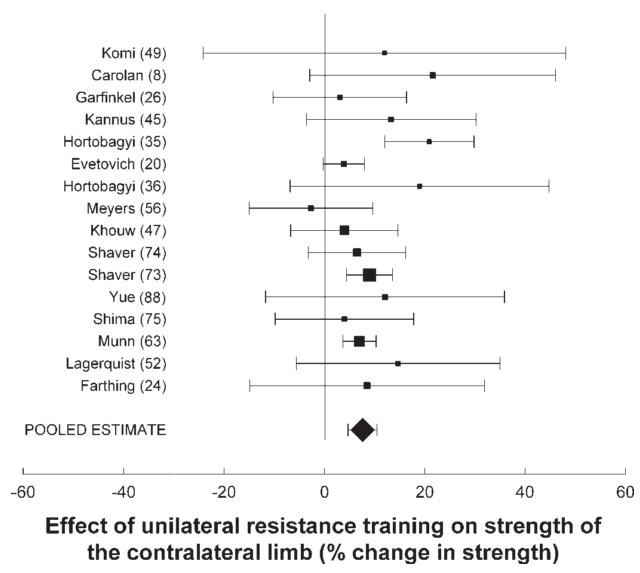
It has been demonstrated in rabbit models that unilateral tendon loading leads to bilateral tendinopathic changes (increase tenocyte size/#, increased proteoglycan content, neovascularization). It has also been demonstrated that human subjects with unilateral tendinopathy display bilateral sensory/motor deficits. This leads us to the possibility that central mechanisms may be influencing these bilateral effects. This central effect, termed the “Crossover Phenomenon,” was first described over 100 years ago by Scripture et al. out of the Yale Psychology Lab. In this study, the subject performed 10 maximum repetitions of a squeeze bulb (baseline strength for both hands).  10 maximum repetitions were performed on 8 different sessions over a 2-week period on the RIGHT hand only. At the end of the 2-week training period, the strength of both hands was measured, which yielded a 43% increase in strength of the LEFT (untrained!) hand! The strength of the right hand was significantly higher, yet the untrained arm experienced a very meaningful improvement. Since 1894, this phenomenon has been studied in many settings. A 2006 meta-analysis by Carrol et al. looked at studies investigating this phenomenon and found increases in the contralateral (untrained limb) averaged 7.6%, which represented a 52% increase compared to the ipsilateral (trained limb) side. Put another way, if I train my right bicep to curl 20 extra pounds over a given period, the left arm will be able to curl an additional 10 pounds without even training!
10 maximum repetitions were performed on 8 different sessions over a 2-week period on the RIGHT hand only. At the end of the 2-week training period, the strength of both hands was measured, which yielded a 43% increase in strength of the LEFT (untrained!) hand! The strength of the right hand was significantly higher, yet the untrained arm experienced a very meaningful improvement. Since 1894, this phenomenon has been studied in many settings. A 2006 meta-analysis by Carrol et al. looked at studies investigating this phenomenon and found increases in the contralateral (untrained limb) averaged 7.6%, which represented a 52% increase compared to the ipsilateral (trained limb) side. Put another way, if I train my right bicep to curl 20 extra pounds over a given period, the left arm will be able to curl an additional 10 pounds without even training!
So what are the potential mechanisms which could explain this phenomenon and how could we use this to our advantage with our athletes and patients? There are several neuroanatomical pathways which connect the left and right side of our body, facilitating basic human functions such as walking. These pathways include commissural interneurons in the spinal cord, and a host of inter-hemispheric connections in the cerebral cortex.
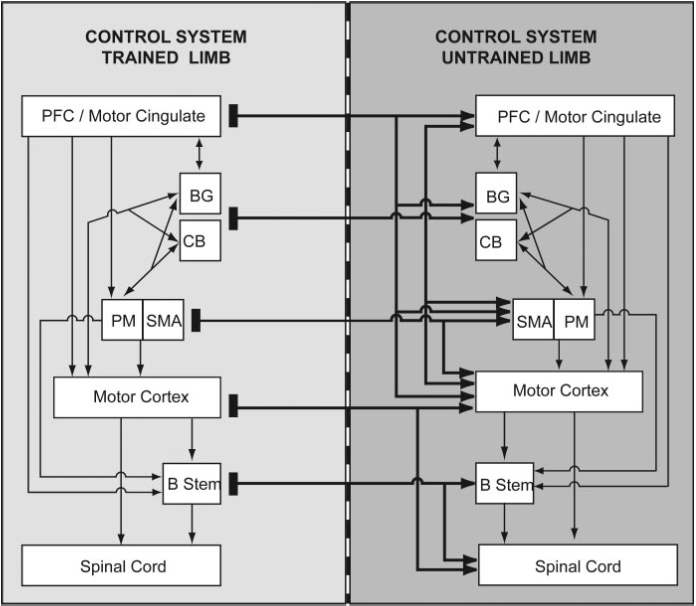
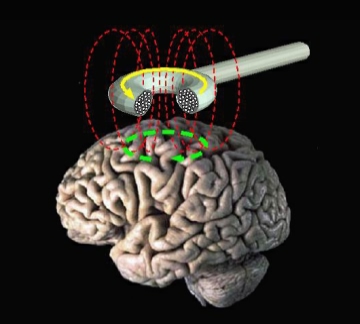
These cross connections can be tested using transcranial magnetic stimulation (TMS), a brain-stimulation technique that uses magnetic impulses in the cerebral cortex to induce a motor response. Descending pyramidal pathways, which cross to the opposite side of the body, control areas of the motor cortex based on the topographical configuration known as the motor homunculus. The output of the stimulation can be measured and gives a direct quantification of motor control (more in Part 2).
So now that we’ve laid some preliminary groundwork for understanding the central mechanisms that may be involved in tendinopathy, what can we do with this information? TNT proposes that combining an external cue with isotonic/isometric strength training can modulate the motor control deficits seen in tendinopathy that may not be adequately addressed by standard treatments (NSAIDs, passive modalities, eccentric exercise). In order to perform this technique, download a free metronome app (e.g. ProMetronome). Set the BPM to 20 (1 every 3 seconds). Pace your exercise such that you have a 3-second concentric and 3-second eccentric contraction and perform 8 repetitions. 6-seconds x 8 reps = 48 seconds (previous research suggests a 45-second time under tension). While the exact frequency, intensity, duration, and type of exercise are up for debate, the research suggests 4 sets (2-minute rest), 3 days per week. Regarding the tendinopathy research, and in our experience, the duration of the program would need to be at least 4 weeks (more likely 8), but may need to be longer (4-12 weeks, 15-48 sessions, 55-100% 1RM).

Some other considerations for this technique:
- As previously mentioned, the exact frequency, intensity, time, and type of exercise is not completely known. Future research can better define these parameters and compare efficacy to other interventions.
- In the case of a highly painful unilateral tendinopathy, could the patient perform TNT on the opposite limb with the intent of affecting the painful side via the crossover phenomenon?
- Would complex and variable movements (with greater cortical activation) yield additional benefits compared to a single exercise choice aimed at loading the target tendon?
- What is the exact role of the visual stimulus? Do specific eye movements alter outcomes and should we be mindful of which visual field we choose to monitor the visual cue?
- Is there benefit to task specificity? Again, optimal exercise choice is not yet known.
In Part 2 of this series, we will further review the concept of motor control, which is a central tenet of the AMA paradigm. Labeling something as a motor control “dysfunction” requires an understanding of the mechanisms that can contribute to this system. At AMA, we ascribe to the notion that if you don’t understand (or try to understand) the underlying mechanisms of your intervention, you might as well be guessing!
Patrick Welsh, BSc, DC, FRCCSS(C)
Co-Director of AMA
References:
Carroll TJ, Herbert RD, Munn J, Lee M, Gandevia SC, Timothy J. Contralateral effects of unilateral strength training : evidence and possible mechanisms. J Appl Physiol. 2006;101(5):1514-1522. doi:10.1152/japplphysiol.00531.2006.
Docking SI, Ooi CC, Connell D. Tendinopathy: Is Imaging Telling Us the Entire Story? J Orthop Sport Phys Ther. 2015;45(11):842-852.
Miniaci A, Mascia AT, Salonen DC, Becker EJ. Magnetic resonance imaging of the shoulder in asymptomatic professional baseball pitchers. Am J Sports Med. 2002;30(1):66-73.
Paavola M, Kannus P, Paakkala T, et al. Long-term prognosis of patients with Achilles tendinopathy. An observational 8-year follow-up study. Am J Sports Med. 2000;28:634–42.
Rio E, Kidgell D, Moseley GL, Cook J. Elevated corticospinal excitability in patellar tendinopathy compared with other anterior knee pain or no pain. Scand J Med Sci Sports.
Rio E, Kidgell D, Moseley GL, et al. Tendon neuroplastic training: changing the way we think about tendon rehabilitation: a narrative review. Br J Sports Med. 2015;50:209-215.
Scripture EW, Smith TL, Brown EM. On the education of muscular control and power. Stud from Yale Psychol Lab. 1894;2:114-119.
Welsh P. Tendon neuroplastic training for lateral elbow tendinopathy : 2 case reports. J Can Chiropr Assoc. 2018;62(2):98-104.
